Healthcare in India: Futuristic Vision to Social Development
- In Economics
- 10:44 AM, Sep 12, 2020
- Pankaj Kumar
Introduction
With a population of 1.37 billion, India is the second largest populated country; with a projected growth rate at 1.1%, some experts claim that India will surpass China by 2027. India, the fastest growing trillion-dollar economy surpassed United Kingdom and France in 2019 with a nominal GDP of $2.94 trillion and $10.51 trillion in terms of purchasing power parity. Several studies suggest that India’s growth rate should stabilise at 8% during the next decade making it the world’s fastest-growing economy. Its GDP could overtake that of the US before 2050, turning India into the strongest economy worldwide.
The economic growth over two decades has definitely contributed in reduction of mass poverty and has shown considerable growth in other factors of the well-being but it still lags behind in access to education and healthcare. To address these “failures” the Indian government announced an exceptional National Health Protection Scheme (NHPS), or in Hindi, the Ayushman Bharat Yojana (popularly known as “Modicare”), designed to provide health insurance coverage to roughly 100 million “poor and helpless families” (or an estimated 500 million individuals) in the Year 2018 based on the recommendation of the National Health Policy 2017; with an aim to provide Universal Health Coverage to citizens of India. Under this, two inter-connected components were envisaged namely, Health & Wellness Centres and National Health Protection Scheme.
Ayushman Bharat - National Health Protection Mission will target about 10.74 crore poor, deprived rural families and identified occupational category of urban workers' families as per the latest Socio-Economic Caste Census (SECC, 2011) data covering both rural and urban areas. The scheme is designed to be dynamic and aspirational and it would take into account any future changes in the exclusion/ inclusion/ deprivation/ occupational criteria in the SECC data.
World Bank (WB) and World Health Organization (WHO) report 2017 states, more than half of the world’s 7.7 billion population, do not have access to the basic health care services. 60 million people are pushed into poverty every year due to rising health spending, and the impact of health spending on poverty is very high. About 97 million people were impoverished due to spending on health care in 2010. Globally, an estimated 588 million (9.7%) people had incurred Catastrophic Health Spending (CHS) in 2000 and it has increased to 808 million (11.7%) in 2010. All these vulnerable families spend more than 10% of their earnings every year on medical treatment of family members and their dependants.
According to the World Bank report, the total expenditure on health care as a proportion of GDP in 2016 was 18% with the United States topping the list. Out of this, the government’s health expenditure as a proportion of GDP is just 10.02%, and the out-of-pocket expenditure as a proportion of the current health expenditure was 33% in 2016.
India’s National Health Policy, 2017 envisages raising public health expenditure to 2.5% of GDP by 2025 in a time bound manner. It also envisages increasing state sector health spending to more than 8% of their budget by 2020. NHP-2017 has its goal fully aligned with the concept of Universal Health Coverage which is with reference to the Goals of WHO SDGs (Sustainable
Development Goal) and its commitment, which is to “leave no one behind” of year 2015 which is aimed to be achieved by year 2030.
Source - Ayushman Bharat
Indian Health sector has witnessed various reforms in the last 2 decades such as: institutionalising of IRDA, inviting the private players in the insurance market, progression in health insurance premium, de-tariffication, introduction of TPAs, cashless hospitalization benefits, surge in health insurance claim ratio, formation of standalone health insurance companies, unveiling of innovative health insurance products, increase in healthcare cost, minor improvements in the health indicators at the country level, launch of government funded policy for the poor’s and increase in the number of cases going to insurance ombudsman and recently the stopping of cashless facility by the PSU insurers.
There are numerous initiatives which has been taken in the domain of health but it seems to be not mitigating the proportion, thereby leaving the population to suffer enmasse.
Ironically, the Indian health industry is expected to reach ₹19,56,920/- crore by 2020 and is one of the popular destinations for medical tourism.
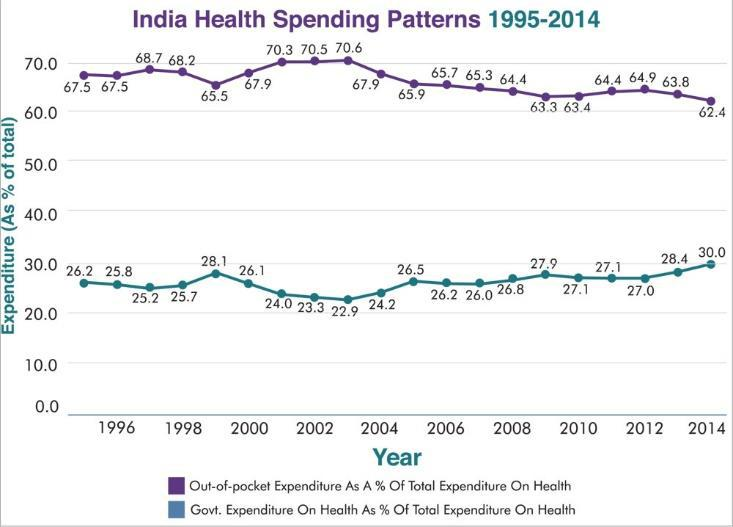
The way in which Indian healthcare is financed is critical for equity in access to healthcare. At present the proportion of public resources committed to healthcare in India is one of the lowest in the world, with less than one‐fifth of health expenditure being publicly financed. India has large‐scale poverty and yet the main source of financing healthcare is out‐of‐ pocket expenditure. This is a cause of the huge imbalances we see in access to healthcare.
References:
Tyroler, H., (et al) (1965). Patterns of Preventive Health Behavior in Populations. Journal of Health and Human Behavior, 6(3), 128-140.
Andersen, R., & Newman, J. (1973). Societal and Individual Determinants of Medical Care Utilization in the United States. The Milbank Memorial Fund Quarterly. Health and Society, 51(1), 95-124.
Rosenstock, I. M. (1974). Historical Origins of the Health Belief Model. Health Education Monographs, 2(4), 328–335.
Mark T, Sree S, The modern mental health system in Nepal: Organizational persistence in the absence of legitimating myths, Social Science & Medicine, Volume 45, Issue 3, 1997, Pages 441-447, ISSN 0277-9536
Chakraborty N., (et al), Determinants of the use of maternal health services in rural Bangladesh, Health Promotion International, Volume 18, Issue 4, December 2003, Pages 327–337
Asada, Y., Kephart, G. Equity in health services use and intensity of use in Canada. BMC Health Serv Res 7, 41 (2007).
Duggal, R. (2007), Healthcare in India: Changing the Financing Strategy. Social Policy & Administration, 41: 386-394.
DALE V., Humanism: A Theoretical Perspective, The Journal of Humanistic Education and Development, 21, 3, (101-106), (2011)
Lahana, E., (et al) (2011). Do place of residence and ethnicity affect health services utilization? Evidence from Greece. International journal for equity in health, 10, 16.
Li, L., (et al) (2012), Chinese Healthcare Reform. Modern China, 38(6), 630-645.
Molina-Aguilera IB, (et al), integrating health promotion and disease prevention interventions with vaccination in Honduras. J Infect Dis. 2012 Mar; 205 Suppl 1:S77-81
Sommers B. Obamacare’s 2014 report card? Preaching patience — to supporters and opponents. Harvard Public Health Review. Spring 2014;
Mohanty, S.K., (et al). Out-of-pocket Expenditure on Health Care among Elderly and Non-elderly Households in India. Soc Indic Res 115, 1137–1157 (2014).
Sen A. Universal health care: the affordable dream. Harvard Public Health Review. Spring 2015; 5.
Sharma S. Health care for India’s 500 million: the promise of the National Health Protection Scheme. Harvard Public Health Review. Fall 2018; 18.
Lahariya, C. ‘Ayushman Bharat’ Program and Universal Health Coverage in India. Indian Pediatr 55, 495–506 (2018)
Garg S. Universal health coverage in India: Newer innovations and the role of public health. Indian J Public Health [serial online] 2018
Chhabra, S., (et al), 2018, India - Case Study on Institutional Arrangement for Detecting Fraud in Government Health Insurance Program: Anti-Fraud Efforts in Government-Sponsored
Health Insurance Schemes in Four Indian States (English). Washington, D.C.: World Bank Group.
Tabish, S A. (2018). TRANSFORMING HEALTH CARE IN INDIA: AYUSHMAN BHARAT-NATIONAL HEALTH PROTECTION MISSION. International Journal of Scientific Research. 7. 16-25.
Angell BJ, (et al) (2019), The Ayushman Bharat Pradhan Mantri Jan Arogya Yojana and the path to universal health coverage in India: Overcoming the challenges of stewardship and governance. PLoS Med 16(3): e1002759.
Dhankhar A. Ayushman Bharat, one year on: Big challenges and bigger opportunities lie ahead of govt's flagship programme, FP-2019, 10
Choudhury, M., (et al), 2019. "Private Hospitals in Health Insurance Network in India: A Reflection for Implementation of Ayushman Bharat," Working Papers 19/254, National Institute of Public Finance and Policy.
Cicinelli, M. V., (et al) (2020). Comprehensive eye care - Issues, challenges, and way forward. Indian journal of ophthalmology, 68(2), 316–323.
Department of Industrial Policy and Promotion (DIPP), RNCOS Reports, Media Reports, Press Information Bureau (PIB)
Access to Health Care and Community Social Capital. (2020). Retrieved 27 February 2020
Image Credits: Wion News






Comments